What’s the Deal with the Prostate?
Let’s talk about Prostate Ailments. The Prostrate Gland is this little organ that’s part of the male reproductive system, but it often flies under the radar until something goes wrong. Tucked away below the bladder and surrounding the urethra, this walnut-sized wonder plays a crucial role in reproduction and urination. But what exactly does it do, and why should we care about it? Let’s dive in and explore the ins and outs of this mysterious gland.
Location and Size:
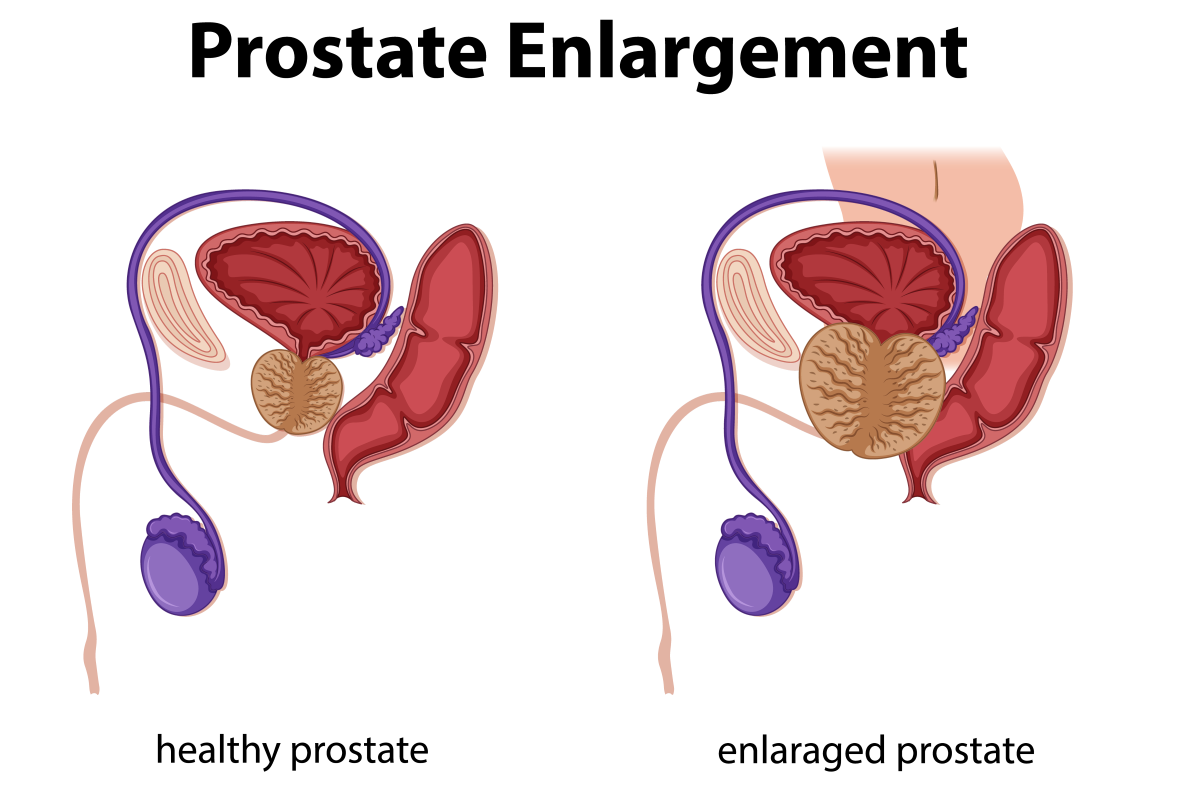
Where’s Waldo, but for Your Body Picture this: you’re on a treasure hunt inside the male body. Your mission? Find the prostate. Head south from the bladder, and you’ll spot it wrapped around the urethra like a tiny donut. It’s about the size of a walnut in young men, but don’t be fooled – this little guy tends to grow as you age. By the time a man hits his 70s, it might be more like a lemon. Talk about a growth spurt!

Function:
The Multitasking Marvel Now, you might be wondering, “What’s the point of this little gland?” Well, it’s quite the multitasker. First off, it’s a key player in the baby-making game. The prostate produces a fluid that makes up about 30% of semen, helping those swimmers reach their destination. But that’s not all – it also acts like a gatekeeper, controlling the flow of urine and semen. It’s like a traffic controller for your nether regions.
Common Problems:
When Things Go South Like any body part, the prostate can sometimes cause trouble. As men age, they might face a few common issues. There’s benign prostatic hyperplasia (BPH), where the prostate decides to supersize itself, making peeing a real challenge. Then there’s prostatitis, which is just a fancy way of saying the prostate gets inflamed and angry. And let’s not forget about prostate cancer – it’s the second most common cancer in men worldwide.
Symptoms:
Listen to Your Body So how do you know if your prostate is trying to tell you something? Well, it’s all about paying attention to the signs. Having trouble starting or stopping your pee stream? Feeling like you need to go all the time, especially at night? Experiencing pain or burning when you urinate? These could all be your prostate’s way of waving a red flag. Don’t ignore these symptoms – they’re worth a chat with your doc.
Prevention and Care:
Treat Your Prostate Like a VIP Taking care of your prostate isn’t rocket science, but it does require some effort. Regular check-ups with your doctor are a must, especially as you get older. They might recommend screening tests like the PSA blood test or a digital rectal exam (yeah, it’s not the most fun, but it’s important). Eating a healthy diet, staying active, and managing stress can all help keep your prostate happy. Think of it as a little thank-you gift for all the hard work it does.
Research and Future:
The Prostate Frontier Scientists are always on the hunt for new ways to understand and treat prostate issues. From developing better screening methods to exploring cutting-edge treatments, the world of prostate research is buzzing with activity. Who knows? In a few years, we might have even more tools to keep this tiny but mighty gland in tip-top shape. The future of prostate health is looking brighter than ever.
Prostate Ailments
Benign Prostatic Hyperplasia (BPH)
Benign Prostatic Hyperplasia, or BPH for short, is like your prostate decided to go on an unplanned growth spurt. It’s not cancer, but it can sure cause a lot of trouble. Imagine trying to squeeze toothpaste through a partially pinched tube – that’s kind of what happens when you try to pee with BPH.
As men get older, it’s pretty common for the prostate to enlarge. It’s like the body’s way of saying, “Hey, remember me? I’m still here!” But this growth can put pressure on the urethra, making it harder to empty your bladder. You might find yourself making more trips to the bathroom, especially at night when you’d rather be catching some Z’s.
The symptoms of BPH can be a real pain in the… well, you know. You might notice a weak urine stream, like trying to water plants with a kinked hose. Or maybe you feel like you never quite finish peeing, leaving you with that annoying “gotta go” feeling. Some guys even have trouble starting to pee – talk about performance anxiety!
Are There Ways to Manage BPH?
But don’t worry, there are ways to manage BPH. Doctors might suggest lifestyle changes, like cutting back on coffee (I know, the horror!) or avoiding fluids before bedtime. There are also medications that can help shrink the prostate or relax the muscles around it. In more severe cases, there are surgical options to remove the extra prostate tissue.
Living with BPH can be frustrating, but it’s important to remember that it’s not a life-threatening condition. Still, it’s crucial to get checked out if you’re having symptoms. Not only can treatment improve your quality of life, but it also rules out more serious conditions like prostate cancer. So don’t be shy – talk to your doctor if your prostate’s giving you grief. Your bladder (and your sleep schedule) will thank you!
Prostatitis
Prostatitis is like your prostate threw a tantrum and decided to get all inflamed and angry. It’s a condition that can sneak up on you, causing a world of discomfort in your nether regions. Unlike its cousin BPH, prostatitis doesn’t discriminate by age – it can affect men of all ages, from young bucks to seasoned gents.
There are two main types of prostatitis: bacterial and non-bacterial. Bacterial prostatitis is like having an unwelcome guest crash your prostate party. It’s caused by bacteria that find their way into the prostate, setting up shop and causing inflammation. This type can come on suddenly (acute) or hang around for a while (chronic).
NBP Can Occur Suddenly Without Underlying Reasons
Non-bacterial prostatitis, on the other hand, is a bit of a mystery. It’s like your prostate is throwing a fit for no apparent reason. Doctors aren’t always sure what causes it, but stress, nerve damage, or even a previous urinary tract infection might be to blame.
The symptoms of prostatitis can make you feel like you’re starring in your own personal horror movie. You might experience a burning sensation when you pee (ouch!), feel like you need to go all the time, or have pain in your lower back or pelvic area. Some guys even report pain in their testicles or penis. And if you’ve got the bacterial type, you might feel like you’ve been hit by a truck, with fever, chills, and body aches.
This Can Be Difficult To Diagnose
Diagnosing prostatitis can be tricky, as the symptoms often overlap with other conditions. Your doctor might need to play detective, ordering urine tests, blood tests, or even a prostate massage (yep, that’s a thing) to get to the bottom of it.
Treatment depends on the type of prostatitis you’re dealing with. For bacterial prostatitis, antibiotics are the go-to weapon. Non-bacterial prostatitis might require a combination of approaches, including anti-inflammatory drugs, alpha-blockers to help with urination, or even lifestyle changes like avoiding spicy foods or caffeine.
Living with prostatitis can be challenging, but remember, you’re not alone. Many men deal with this condition, and with proper treatment and management, you can get back to feeling like yourself again. Don’t suffer in silence – reach out to your doctor if you’re experiencing symptoms. Your prostate (and your sanity) will thank you!
Chronic Prostatitis / Chronic Pelvic Pain Syndrome (CP/CPPS)
Chronic Prostatitis / Chronic Pelvic Pain Syndrome, or CP/CPPS for short, is like the Sherlock Holmes of prostate conditions – it’s a real mystery. This sneaky condition causes ongoing pelvic pain and urinary issues, but unlike other forms of prostatitis, there’s no clear infection to blame. It’s like your body’s playing a frustrating game of “Whodunit?” with no clear culprit.
CP/CPPS is actually the most common form of prostatitis, affecting up to 10-15% of the male population. But don’t let that statistic fool you – it’s also one of the most challenging urological conditions to diagnose and treat. It’s like trying to hit a moving target while blindfolded.
What Are The Range Of Symptoms?
The symptoms of CP/CPPS can be a real mixed bag. You might experience pain in your lower abdomen, groin, or back. Some guys report pain in their penis or testicles, which can really put a damper on your love life. Urinary problems are also common – you might feel like you need to pee all the time, or experience burning or pain when you do go. And just to add insult to injury, some men also deal with sexual dysfunction.
What makes CP/CPPS particularly tricky is that these symptoms can come and go. You might have good days and bad days, making it hard to pin down the problem. It’s like playing whack-a-mole with your symptoms.
Diagnosing CP/CPPS is no walk in the park. Doctors often have to rule out other conditions first, like urinary tract infections or other forms of prostatitis. They might run a series of tests, including urine and blood tests, or even do imaging studies. But often, the diagnosis comes down to the pattern of symptoms and ruling out other possibilities.
This Can Be Complicated To Treat And Manage Symptoms
Treatment for CP/CPPS is all about managing symptoms and improving quality of life. It often requires a multi-pronged approach, kind of like assembling your own personal A-Team to tackle the problem. This might include medications like alpha-blockers or anti-inflammatories, physical therapy to relax pelvic muscles, stress management techniques, or dietary changes.
Living with CP/CPPS can be frustrating and sometimes even isolating. The chronic nature of the condition and the lack of a clear cause can take a toll on your mental health. But remember, you’re not alone in this battle. Support groups and counseling can be valuable tools in your CP/CPPS toolkit.
While CP/CPPS remains a challenging condition, researchers are continually working to better understand and treat it. So don’t lose hope – with patience, persistence, and the right medical team, you can find ways to manage your symptoms and improve your quality of life. Your prostate might be giving you grief, but you’ve got the power to fight back!
Acute Bacterial Prostatitis
Acute bacterial prostatitis is like your prostate suddenly caught on fire. It’s a nasty bacterial infection that comes on fast and hits hard. Imagine waking up one day feeling like you’ve been hit by a truck, and your nether regions are staging a full-scale revolt. That’s acute bacterial prostatitis for you.
This condition doesn’t mess around. The symptoms are intense and usually impossible to ignore. You might spike a high fever, feeling like you’re burning up from the inside out. Chills often accompany this, making you feel like you’re on a rollercoaster of hot and cold. And let’s not forget the main event – peeing becomes a whole new adventure, and not the fun kind. It might burn like you’re passing hot lava, or you might struggle to empty your bladder completely.
Did You Know Bacteria Is A Common Cause For This?
The culprits behind this bacterial invasion are often the usual suspects – E. coli or other bacteria that normally hang out in your gut. Sometimes, they take a wrong turn and end up in your prostate, throwing a wild party that your body definitely didn’t RSVP for.
Diagnosing acute bacterial prostatitis is usually straightforward due to the severe symptoms. Your doctor will likely run some tests, including urine and blood cultures, to identify the bacterial troublemakers.
Treatment is a race against time. Antibiotics are the heavy artillery in this battle, often given intravenously in severe cases. You might need to be hospitalized to ensure the infection doesn’t spread to your bloodstream. Pain relief and plenty of fluids are also crucial parts of the treatment plan.
The good news? With prompt treatment, most men recover fully from acute bacterial prostatitis. But it’s not something to take lightly – if you suspect you’ve got it, don’t try to tough it out. Get to a doctor pronto. Your prostate (and the rest of your body) will thank you for the swift action!
Chronic Bacterial Prostatitis
Chronic bacterial prostatitis is like having a houseguest that just won’t leave. It’s a persistent or recurrent infection of the prostate that can hang around for months or even years. Unlike its acute cousin, chronic bacterial prostatitis is more of a slow burn – less intense, but frustratingly long-lasting.
The symptoms of chronic bacterial prostatitis can be sneaky. They might come and go, making you feel like you’re on a prostate-themed rollercoaster. You could experience mild pain in your lower back, groin, or pelvic area. Urinary symptoms are common too – you might find yourself running to the bathroom more often, or feeling like you never quite empty your bladder. And just when you think it’s gone, bam! The symptoms can flare up again.
If UTIs Keep Showing Up, This Could Be The Cause!
One of the hallmarks of chronic bacterial prostatitis is recurrent urinary tract infections (UTIs). It’s like your urinary system is stuck in a loop, with infections popping up again and again. This can be incredibly frustrating, making you feel like you’re always on antibiotics.
Diagnosing chronic bacterial prostatitis can be tricky. Your doctor might need to play detective, running multiple tests over time to catch the bacteria in the act. They might analyze your urine, blood, or even fluid from your prostate to identify the bacterial culprits.
Treatment for chronic bacterial prostatitis is a marathon, not a sprint. Long-term antibiotics are often the go-to approach, sometimes lasting for several weeks or even months. But it’s not just about killing bacteria – managing symptoms is crucial too. This might involve alpha-blockers to help with urination, anti-inflammatory drugs for pain, or even lifestyle changes like avoiding irritants such as alcohol or spicy foods.
Living with chronic bacterial prostatitis can be challenging. It’s important to stick to your treatment plan and follow up regularly with your doctor. With persistence and the right approach, many men can successfully manage this condition and reduce its impact on their daily lives. Remember, you’re in it for the long haul, but you’re not alone in this fight!
Prostate Cancer
Prostate cancer is the boogeyman of men’s health – often feared, sometimes misunderstood, but always taken seriously. It’s one of the most common cancers in men, especially as they age. Think of it as an unwelcome party crasher that shows up uninvited and can cause a whole lot of trouble if not dealt with promptly.
One of the trickiest things about prostate cancer is that in its early stages, it often has no symptoms at all. It’s like a ninja, silently doing its thing without raising any alarms. This is why regular check-ups and screenings are so important, especially for men over 50 or those with risk factors like family history.
The Symptoms Vary Depending On Severity
As prostate cancer advances, it can start to make its presence known. You might experience difficulty urinating, like a weak stream or trouble starting and stopping. Some men notice blood in their urine or semen – definitely not something to ignore. In more advanced stages, prostate cancer can spread to other parts of the body, potentially causing bone pain, especially in the back, hips, or chest.
Diagnosing prostate cancer usually involves a combination of tests. Your doctor might start with a PSA (Prostate-Specific Antigen) blood test and a digital rectal exam (yes, it’s as fun as it sounds). If these raise suspicions, you might need further tests like a biopsy or imaging studies.
What About Treatment Options?
Treatment for prostate cancer depends on various factors, including the stage of the cancer, your overall health, and your preferences. Options can range from active surveillance (keeping a close eye on slow-growing cancers) to surgery, radiation therapy, or hormone therapy. Each approach has its pros and cons, and it’s a decision that requires careful consideration and discussion with your healthcare team.
Living with a prostate cancer diagnosis can be emotionally challenging. It’s normal to feel scared, angry, or overwhelmed. But remember, prostate cancer is often treatable, especially when caught early. Many men go on to live long, healthy lives after treatment. Support groups and counseling can be invaluable resources during this journey.
The key takeaway? Don’t stick your head in the sand when it comes to prostate health. Regular check-ups and open conversations with your doctor are your best defense against prostate cancer. It might not be the most comfortable topic, but it’s one that could save your life. So man up, get checked, and take charge of your prostate health!
Prostate Abscess
A prostate abscess is like your prostate decided to grow its own unwelcome, pus-filled water balloon. It’s a rare but serious complication of bacterial prostatitis, where a pocket of infected fluid forms within the prostate gland. Think of it as your body’s misguided attempt to wall off an infection, but instead of solving the problem, it creates a whole new one.
The symptoms of a prostate abscess are hard to ignore. You might feel like there’s a flaming golf ball lodged in your pelvis, causing severe pain that makes sitting uncomfortable and walking a chore. High fever is common, often accompanied by chills and sweats that make you feel like you’re on a roller coaster of misery. Urinating becomes a Herculean task – you might feel an urgent need to go, only to struggle with getting the flow started or emptying your bladder completely.
It Can Require Careful Examinations To Diagnose
Diagnosing a prostate abscess requires a keen medical eye. Your doctor might suspect it based on your symptoms and physical exam, but confirming it usually involves imaging studies like a transrectal ultrasound or CT scan. These tests can pinpoint the location and size of the abscess, guiding treatment decisions.
Speaking of treatment, it’s not for the faint of heart. Antibiotics are a must to tackle the underlying infection, but they’re often not enough on their own. The abscess itself needs to be drained, either through a needle guided by ultrasound or, in more severe cases, through surgery. It’s like lancing a boil, but in a much more sensitive area.
Recovery from a prostate abscess can take time, and you’ll need to follow up with your doctor to ensure the infection is completely cleared. While it’s a rare condition, it’s not one to take lightly. If you’re experiencing severe prostate symptoms, especially with a high fever, don’t hesitate to seek medical attention. Your prostate will thank you for not letting things come to a head!
Prostate Stones (Prostatic Calculi)
Prostate stones, or prostatic calculi, are like your prostate decided to start its own rock collection. These tiny mineral deposits form within the prostate gland, ranging from microscopic specks to pebble-sized formations. It’s as if your prostate got inspired by kidney stones and thought, “Hey, I can do that too!”
Most of the time, these little stony squatters are harmless and go unnoticed. Many men have them without ever knowing it – they’re often discovered incidentally during other prostate exams or imaging studies. It’s like finding out you’ve been carrying around a secret rock garden all this time.
However, sometimes these stones decide to make their presence known. Larger stones or a significant number of them can cause symptoms similar to other prostate conditions. You might experience chronic pelvic pain, feeling like you’re sitting on a tiny, angry pincushion. Urinary issues can crop up too – difficulty starting or stopping your stream, or feeling like you need to go more often than usual.
Prostate Stones Increase The Amount Of Bacteria In Your Prostate
One of the trickier aspects of prostate stones is that they can become a breeding ground for bacteria. It’s like they’re setting up a cozy bacteria bed and breakfast in your prostate. This can lead to recurrent infections, making you feel like you’re stuck in a loop of antibiotics and discomfort.
Diagnosing prostate stones usually involves imaging studies like ultrasounds or CT scans. Your doctor might spot them during a routine digital rectal exam if they’re large enough.
Treatment for prostate stones depends on whether they’re causing symptoms. If they’re not bothering you, your doctor might suggest a “watch and wait” approach. But if they’re causing pain or recurrent infections, more active treatment might be needed. This could involve medications to help you pass the stones, or in some cases, minimally invasive procedures to remove them.
Living with prostate stones can be a bit of a balancing act. Staying hydrated and maintaining good prostate health can help prevent new stones from forming. And remember, while they might be a pain in the… prostate, with proper management, you can keep these unwelcome rock visitors from taking over your life!
Prostate Cysts
Prostate cysts are like your prostate decided to grow its own water balloons. These fluid-filled sacs can develop within or on the surface of the prostate gland, ranging from tiny, unnoticeable bubbles to larger pockets that can cause a ruckus in your nether regions.
Most prostate cysts are benign, meaning they’re not cancerous. They’re often discovered by chance during routine prostate exams or imaging studies for other conditions. It’s like finding out you’ve been walking around with a hidden water feature all this time.
The causes of prostate cysts can vary. Some are present from birth (congenital), while others might develop later in life due to blockages in the prostate ducts. Infections or inflammation can also lead to cyst formation. It’s as if your prostate is trying to create its own little swimming pools, but forgot to install the filters.
The Cysts Can Cause Issues With Urination
While many prostate cysts are asymptomatic, larger ones can cause problems. They might press on the urethra or other surrounding structures, leading to symptoms similar to benign prostatic hyperplasia (BPH). You might find yourself making more frequent trips to the bathroom, especially at night. Some men experience difficulty starting or stopping their urine stream, or feel like they can’t empty their bladder completely. It’s like trying to squeeze toothpaste out of a tube that someone’s pinching in the middle.
Diagnosing prostate cysts usually involves imaging studies like transrectal ultrasound or MRI. These tests can help determine the size, location, and nature of the cysts.
Treatment for prostate cysts depends on whether they’re causing symptoms and their size. Small, asymptomatic cysts often don’t need treatment – your doctor might just keep an eye on them during regular check-ups. For larger or symptomatic cysts, drainage might be necessary. This can be done through a needle aspiration guided by ultrasound, or in some cases, through surgery.
While Not Dangerous, They Can Become Infected Or Cancerous
While prostate cysts are generally not dangerous, they can sometimes become infected or, rarely, harbor cancer cells. That’s why it’s important to have regular prostate check-ups, especially if you’re experiencing any urinary symptoms.
Living with prostate cysts is often about management and monitoring. With proper medical care, most men can keep these fluid-filled freeloaders from causing too much trouble. Remember, while they might make your prostate feel like it’s trying to start its own water park, you’ve got the power to keep things under control!

Prostate Nodules
Prostate nodules are like unexpected speed bumps in your prostate highway. These small lumps or bumps can be felt during a digital rectal exam (DRE), causing your doctor’s finger to hit the proverbial brakes. It’s like your prostate decided to grow its own set of worry beads, but instead of bringing calm, they often bring concern.
These nodules can vary in size and texture, ranging from tiny pebble-like bumps to larger, more distinct masses. They’re like the prostate’s way of saying, “Hey, pay attention to me!” And trust me, they definitely get attention from your healthcare provider.
The tricky thing about prostate nodules is that they can mean different things. Sometimes, they’re simply a sign of inflammation or infection, like your prostate’s way of throwing a tiny tantrum. Other times, they might be benign growths, like little prostate pimples that are annoying but harmless. However, in some cases, nodules can be early warning signs of prostate cancer, which is why they’re always taken seriously.
Further Tests Are Necessary As Nodules Can Be Almost Anything
When a nodule is detected during a DRE, it often kicks off a series of further investigations. Your doctor might order blood tests, including a PSA (Prostate-Specific Antigen) test, to check for signs of cancer. Imaging studies like ultrasounds or MRIs might be next on the agenda to get a better look at the nodule’s size, shape, and location. In some cases, a biopsy might be necessary to determine if the nodule is cancerous or benign.
It’s important to remember that finding a nodule doesn’t automatically mean you have cancer. Many nodules turn out to be completely harmless. However, they’re always a signal that your prostate needs some extra attention.
Living with the knowledge of prostate nodules can be anxiety-inducing. It’s normal to feel worried or scared. But remember, early detection is key in managing any potential issues. Regular check-ups and open communication with your healthcare provider are your best tools in navigating the bumpy road of prostate nodules.
So, while these little lumps might feel like unwelcome guests, think of them as your body’s way of saying, “Hey, let’s make sure everything’s okay down here.” It’s not the most comfortable conversation starter, but it’s one that could potentially save your life!
Neurogenic Bladder Associated with Prostate Disease
Neurogenic bladder associated with prostate disease is like your bladder and prostate are trying to play a game of telephone, but the wires got crossed. This condition occurs when nerve damage messes with the communication between your brain, bladder, and prostate, leading to a whole host of urinary issues. It’s as if your plumbing system suddenly decided to ignore the on and off switches.
In a normally functioning system, your brain sends signals to your bladder when it’s time to go, and your bladder responds accordingly. But with neurogenic bladder, this well-choreographed dance gets out of sync. You might feel the urgent need to pee but struggle to actually go, or you might not feel the need at all and suddenly find yourself with wet pants. It’s like your bladder’s playing a cruel game of “Made you look!”
The prostate plays a role in this condition because of its location. Wrapped around the urethra like a donut, the prostate can compound the problems of neurogenic bladder. Prostate enlargement or inflammation can further obstruct urine flow, making the symptoms of neurogenic bladder even more pronounced.
Multiple Tests Are Required To Narrow Down The Cause
Diagnosing neurogenic bladder associated with prostate disease often involves a combination of tests. Your doctor might order urodynamic studies to see how well your bladder is storing and releasing urine. Imaging tests can help visualize your urinary system and prostate. And neurological exams might be needed to check for nerve issues.
Treatment for this condition is often multifaceted. It might involve medications to relax the bladder or shrink the prostate, catheterization to help empty the bladder, or even surgical interventions in severe cases. Pelvic floor exercises, also known as Kegels, can sometimes help improve bladder control.
Living with neurogenic bladder can be challenging. It might mean planning your day around bathroom access or dealing with the anxiety of potential accidents. But with proper management and treatment, many people are able to regain control and improve their quality of life.
Remember, while it might feel like your bladder and prostate are engaged in a frustrating game of miscommunication, you’re not alone in this. With the right medical team and treatment plan, you can work towards getting your urinary system back on the same page!
Post-Prostatectomy Syndrome
Post-prostatectomy syndrome is like the unwelcome after-party following prostate removal surgery. It’s a set of complications that can crash your recovery celebration, bringing with it a host of challenges that can impact your quality of life. Think of it as your body’s way of saying, “Hey, remember that prostate you got rid of? Well, we’re still adjusting to its absence!”
One of the most common issues in this syndrome is erectile dysfunction. It’s like your love life suddenly hit a speedbump. The nerves responsible for erections run close to the prostate, and they can be damaged during surgery. For some men, it’s a temporary setback, while for others, it might require long-term management with medications or other treatments.
Did You Know This Can Affect Your Bladder Control?
Incontinence is another frequent party crasher in post-prostatectomy syndrome. You might find yourself leaking urine when you laugh, sneeze, or exercise. It’s as if your bladder decided to play a practical joke on you. For most men, this improves over time, but it can be frustrating and embarrassing in the meantime.
Perhaps the most psychologically challenging aspect for many men is the potential for a shortened penis. Yes, you read that right. After prostate removal, some men notice their penis seems shorter. It’s not that it actually shrunk, but rather that the urethra was shortened when the prostate was removed, causing the penis to retract a bit. It’s like your body’s playing a cruel game of “now you see it, now you don’t.”
Can It Affect My Sexual Activity?
Other potential issues include changes in orgasm sensation (you might experience “dry” orgasms), loss of fertility, and in some cases, chronic pain. It’s like your body’s trying to rewrite the owner’s manual, but forgot to give you the updated version.
Dealing with post-prostatectomy syndrome often requires a multidisciplinary approach. You might work with urologists, physical therapists, and even mental health professionals to address the various aspects of the syndrome. Treatments can range from medications and pelvic floor exercises to more advanced options like penile implants for severe erectile dysfunction.
Living with post-prostatectomy syndrome can be challenging, both physically and emotionally. It’s normal to feel frustrated, angry, or depressed. But remember, many men successfully navigate these waters and go on to lead fulfilling lives. Support groups can be invaluable, providing a space to share experiences and coping strategies with others who truly understand.
While post-prostatectomy syndrome might feel like an uninvited guest at your recovery party, with patience, proper care, and support, you can learn to manage its effects and reclaim your quality of life. It’s a journey, not a sprint, so be kind to yourself along the way!


